-50% less incidence of disease progression in the NK cell-administered patient group than in the non-administered patient group
-Professor Kyuhyung Lee and a joint research team at Asan Medical Center in Seoul conducted phase 2 randomized clinical trials
-Published in ‘Lukemia (citation index 12.897)’, the most prestigious journal in the field of blood cancer
[헤럴드경제=김태열 건강의학 선임기자] Among blood diseases, acute myelogenous leukemia and myelodysplastic syndrome do not respond well to anticancer drugs and occur frequently even after bone marrow transplantation, making it difficult to expect a good prognosis. A recent study has shown that transplanting bone marrow from parents or children to these patients followed by natural killer (NK) cells from the same family reduces the possibility of disease progression.
NK cells are a type of white blood cell in the blood and are the cells that protect the front line of the immune system. Because it recognizes and kills cancer stem cells, the source of cancer cells, without any other stimulation, it is attracting attention as a next-generation immunotherapy approach.
Seoul Asan Hospital Hematology Professor Kyu-Hyung Lee, Korea Institute of Bioscience and Biotechnology Research Honorary Researcher In-Pyo Choi (Chief Research Officer, Ingenium Therapeutics), and KAIST Professor Kwang-Hyun Jo of the Department of Brain Biosciences and Engineering hosted parent-child bone marrow transplantation for acute myelogenous leukemia and myelodysplasia syndrome As a result of NK cell donation from bone marrow donors to patients who received
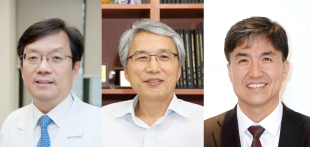
| [사진] (From left) Professor Kyu-hyung Lee of the Department of Hematology of Asan Medical Center, Honorary Researcher In-pyo Choi of the Korea Bioscience and Biotechnology Research Institute, and Professor Gwang-hyeon Cho of the Department of Brain Biosciences and Engineering at KAIST |
This study is significant in proving that NK cell therapy is effective in blood diseases that tend to recur or are classified as high risk, and presents an alternative to refractory cancer treatment. There have been similar studies abroad, but this is the first study conducted based on a randomized control method with a high level of evidence.
The research team recruited 76 participants for the trial between 2015 and 2018. All participants were half-matched bone marrow transplant patients who underwent a parent-child bone marrow transplant for acute myeloid leukemia and myelodysplastic syndrome.
Although the incidence of acute myeloid leukemia and myelodysplastic syndrome is increasing rapidly as the population ages, leukemia cells are known to be resistant to anticancer drugs and treatment effects are difficult to see in most patients even if a bone marrow transplant is done.
The research team randomly assigned participants to an NK cell administration group (40 people) and a control group (36 people). To the NK cell administration group, bone marrow donor-derived NK cell therapy was administered twice over 2 to 3 weeks after bone marrow transplantation, and blood lymphocyte counts and cytotoxicity were measured regularly to determine changes in immunological status following treatment. . The observation period was 30 months until September 2020, during which time the disease developed in 35% of the administered group and 61% of the non-administered group, showing a large difference of around 50% between the two groups.
At 3 months after bone marrow transplantation, the average number of NK cells and T cells was measured to examine the degree of immune recovery. There were 57 refractory patients with very low treatment effects at the time of semi-concordant bone marrow transplantation, and among them, 77% of the administered group and 52% of the non-administered group showed complete remission.
The research team analyzed the mechanism of action by single-cell RNA sequencing (scRNA-seq), and confirmed that memory-like NK cells increased 34-fold in the NK-cell-administered group compared to the group that did not. administered. Additionally, the increase in pseudo-memory NK cells was found to increase anticancer efficacy by proliferating the patient’s memory CD8 T cells.
Lee Kyu-hyung, professor of hematology at Asan Medical Center, said, “Through this study, we were able to clinically confirm the effectiveness of NK cells in refractory blood diseases. We will continue research into developing treatments that use NK cells for many patients who have not been able to receive additional treatment.”
Choi In-pyo, an honorary researcher at the Korea Bioscience and Biotechnology Research Institute, said, “This study was conducted as an investigator-led phase 2 clinical trial, and we are currently preparing a phase 2 clinical trial for NK cell therapy in three domestic medical organization targeting patients with acute myeloid leukemia for conditional approval of NK cell therapy. does,” he said.
Meanwhile, since the early 2000s, the research team has been developing a key source technology for the differentiation and proliferation of NK cells from peripheral monocytes, and was able to obtain approximately 10 times more NK cells than on previously obtained. This technology was recently transferred to Ingenium Therapeutics Co, Ltd and is preparing for commercialisation.
kty@heraldcorp.com