Interview Summary
Ozanimod is a sphingosine 1-phosphate (S1P) receptor modulator indicated for the treatment of relapsing forms of multiple sclerosis (RMS), including clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults. Contraindications for ozanimod include patients who, in the last 6 months, experienced myocardial infarction, unstable angina, stroke, transient ischemic attack, decompensated heart failure requiring hospitalization, or Class III/IV heart failure, or have a presence of Mobitz Type II second-degree or third-degree atrioventricular block, sick sinus syndrome, or sino-atrial block, unless the patient has a functioning pacemaker; patients with severe untreated sleep apnea; or patients taking a monoamine oxidase (MAO) inhibitor. The molecular structure of ozanimod is distinct from that of earlier S1P receptor modulators, such as fingolimod, and binds with high affinity to S1P1 and S1P5. Experts regina Berkovich, founder and Director of the Berkovich MS Center and Research Institute and nationally recognized multiple sclerosis (MS) specialist based in West Hollywood, California, USA; and Robert Shin, Professor of Neurology and Ophthalmology at the University of Virginia, Charlottesville, and Director of the UVA Multiple Sclerosis and Clinical Neuroimmunology Center, USA, discussed several aspects of ozanimod therapy. Thay discussed ozanimod’s molecular structure, which distinguishes it from earlier S1P modulators, and reviewed long-term safety data (up to 7 years) from the DAYBREAK open-label extension (OLE) study and real-world evidence (RWE), including rates of serious adverse events (AE), infections, and treatment discontinuations. they described ozanimod’s efficacy in reducing annualized relapse rates (ARR) and MRI lesion activity in patients with early relapsing MS, and data on 3- and 6-month confirmed disability progression (CDP). shin and Berkovich note how, taken together, these findings show that ozanimod as an oral disease-modifying therapy (DMT) might potentially be suitable for early intervention in adults with relapsing MS.
AN UNMET NEED FOR PATIENTS WITH RELAPSING MULTIPLE SCLEROSIS
MS is a chronic, immune-mediated, central nervous system disorder.1 It involves persistent, low-grade neuroinflammation and recurrent relapses of demyelinating lesions with heterogeneous clinical presentation.1 Relapses in early disease stages are typically followed by partial or full recovery, termed remission.1 MS is more prevalent in females, and the relapsing-remitting form represents the most common early phenotype, seen in over 90% of cases.1 As patients transition to the secondary progressive phase, disability gradually accumulates, with or without continuing relapses.1 This disease course underscores the need for early and effective intervention.1
Current therapeutic approaches target three key goals: reducing inflammation, preventing relapses, and delaying progression to secondary progressive MS. DMTs, delivered orally, by injection, or via infusion, suppress or modulate immune activity to achieve these goals.1 Though, Shin highlighted that there is an unmet need for oral DMTs that people with early MS can remain on long-term without interruption by AEs. Despite clear evidence that early treatment improves outcomes,around 20% of patients do not initiate DMT within 6 months of diagnosis.2-4 High-efficacy immunosuppressive therapies, such as anti-cluster ofIn SUNBEAM (n=1,346) and RADIANCE (n=1,313), ozanimod achieved a safety profile comparable to IFN β-1a, with similar rates of infection (35% versus 34%), herpes zoster infections (0.6% versus 0.2%),serious infections (1.0% versus 0.8%),14 and AEs leading to discontinuation for patients treated with 0.92 mg (2.9–3.0% versus 3.6–4.1%).19,21 The most common AEs (with an incidence of at least 2% in ozanimod-treated patients and at least 1% greater than IFN β-1a) were upper respiratory infection (26% versus 23%), hepatic transaminase elevation (10% versus 5%), orthostatic hypotension (4% versus 3%), urinary tract infection (4% versus 3%), back pain (4% versus 3%), hypertension (4% versus 2%), and upper abdominal pain (2% versus 1%).14
A DEEP DIVE INTO THE LONG-TERM SAFETY PROFILE OF OZANIMOD
Shin emphasized that,while ozanimod showed comparable safety and superior efficacy in comparison to IFN β-1a in the pivotal trials,19,21 long-term evaluation remains essential. Both he and Berkovich underscored the importance of patients remaining on effective, well-tolerated DMTs for extended time periods without switching. The DAYBREAK OLE (NCT02576717) evaluated long-term use of ozanimod.22 This single-arm,open-label,Phase III study enrolled patients who completed SUNBEAM or RADIANCE to assess ozanimod’s long-term safety and efficacy. As Shin explained, the objective of an OLE study is “to [determine whether] the safety profile remains good … and efficacy persists over time.” In DAYBREAK, all participants who entered from the preceding Phase III trials underwent dose escalation to ozanimod 0.92 mg once daily, irrespective of their previous treatment assignment, and maintained this dose throughout the study.22
Overall Adverse Events
in the DAYBREAK OLE (n=2,256), 89.0% (n=2,219) of patients reported treatment-emergent AEs (TEAE) (Figure 2A). Of these, 15.3% (n=381) were serious TEAEs; 9.6% (n=240) were severe TEAEs; and 3.9% (n=98) were TEAEs leading to permanent treatment discontinuation.22 TEAEs greater than or equal to 10% were nasopharyngitis (21.3%), headache (17.1%), and COVID-19 (16.5%).22 Similar safety patterns were seen in the continuous ozanimod 0.92 mg oral daily dose (n=881) population.22
Treatment-Emergent infections
Over up to 72 months’ follow-up, treatment-emergent infections generally remained stable or declined over time (Figure 2B), and serious and opportunistic infections remained < 2%; one case of progressive multifocal leukoencephalopathy occurred (Figure 2C).22 Ozanimod may increase the susceptibility to infections, some serious in nature. Life-threatening and rare fatal infections have occurred in patients receiving ozanimod. Consider interruption of treatment with ozanimod if a patient develops a serious infection.14
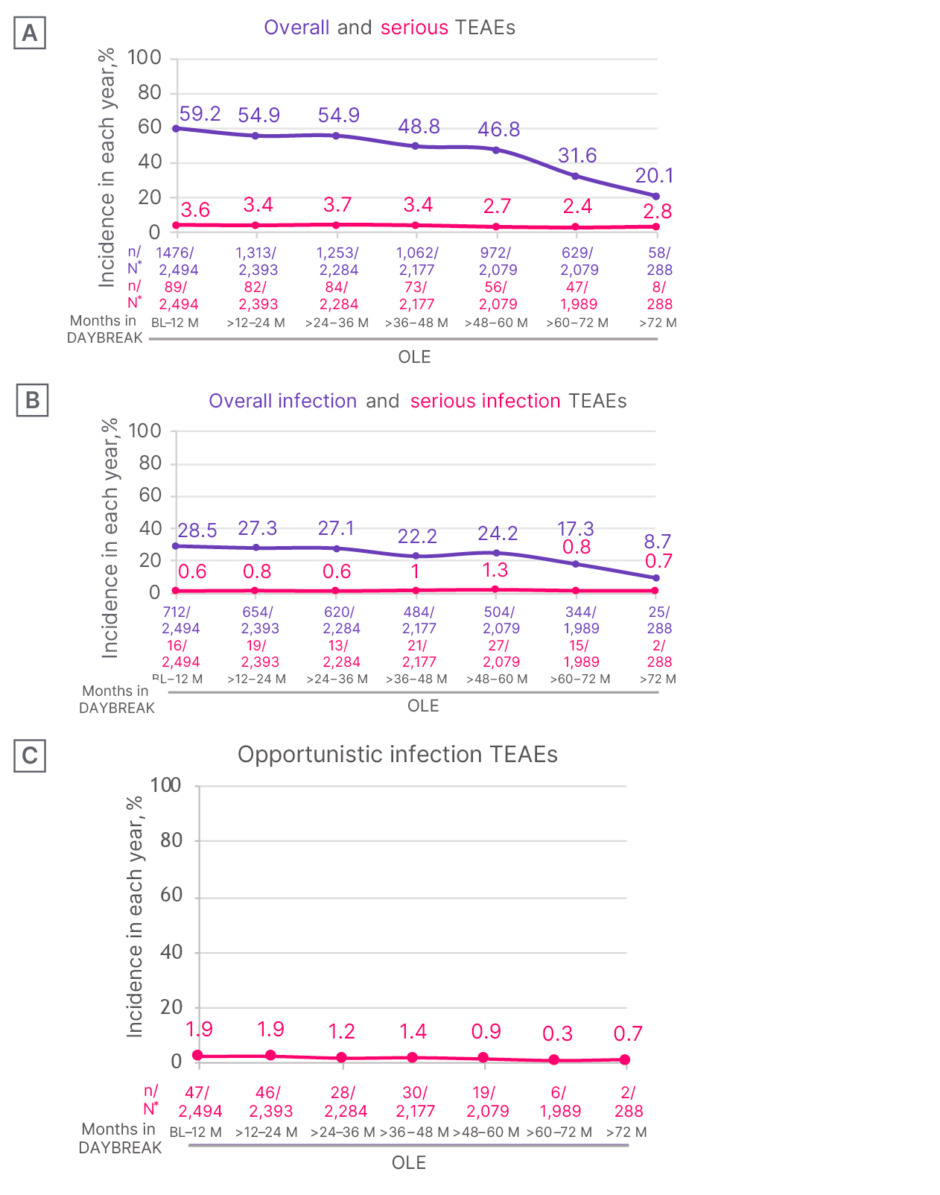
Figure 2: Safety patterns over time with ozanimod during the DAYBREAK open-label extension trial in patients with relapsing multiple sclerosis.22
*Number of participants who had an event in the time interval, divided by the number of participants who were ongoing or discontinued treatment at the same interval; a participant could be counted under multiple time intervals based on the TEAE, TEAE start date, and treatment duration, but if a participant had multiple occurrences of a TEAE in one interval, they were counted once.
Incidence in each year (%) of A) overall and serious TEAEs; and B) overall infection and serious infection TEAEs; C) opportunistic infection TEAEs.
Figure reproduced with permission from Mult Scler.22
M: months; OLE: open-label extension; TEAE: treatment-emergent adverse event.
Absolute Lymphocyte Count and Infection
Absolute lymphocyte count (ALC) was ≥0.5×109 /L in 77% of participants 3 months after the initiation of ozanimod, and remained stable throughout 72 months of follow-up (Figure 3A).23 Patients experienced a mean peripheral blood lymphocyte reduction of approximately 45%. Median time to recovery to normal lymphocyte range was 30 days after ozanimod discontinuation, with 90% of patients with RMS recovering to normal within 3 months.14 Berkovich reiterated that the lymphopenia seen when taking S1P agents “is really artifactual,” referencing the redistribution of lymphocytes from the blood to the lymph nodes.14 In the DAYBREAK OLE study, participants who experienced an initial infection were categorized based on ALC values either at the lab visit prior to the time of first infection or just after the time of first infection. Most patients with any infection had an ALC of between 0.2×109 /L and 0.8×109 /L at the time of first infection, and few patients had an ALC <0.2×109 /L at the time of first infection (Figure 3).24
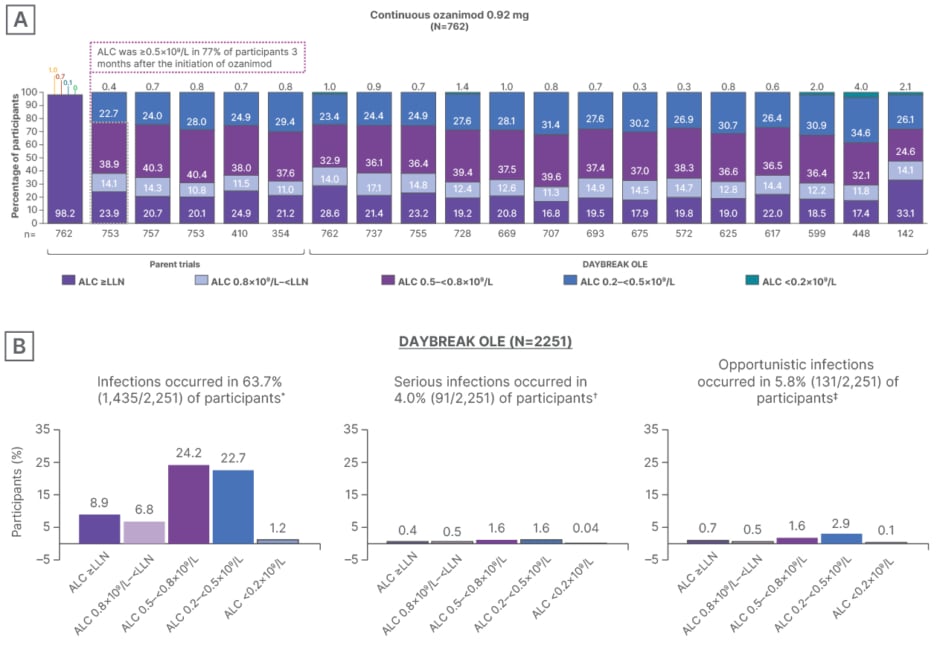
figure 3: Absolute lymphocyte count and infection risk with ozanimod during DAYBREAK open-label extension trial in patients with relapsing multiple sclerosis.23
*Twenty-two participants had an infection with an ALC assessment performed outside of the ±92-day window and were not included in this analysis.
✝Six participants had an infection with an ALC assessment performed outside of the ±92-day window and were not included in this analysis.
‡One participant had an infection with an ALC assessment performed outside of the ±92-day window and was not included in this analysis.
A) ALC with continuous ozanimod from pivotal trials and DAYBREAK OLE. B) Percentage of participants with infections in DAYBREAK OLE (safety population).Participants who experienced an initial infection were categorized based on ALC values either at the lab visit prior to the time of first infection or just after the time of first infection. the minimum ALC is selected if ALC is available both prior to and after the first infection.
Figure reproduced with permission from Selmaj et al.23
ALC: absolute lymphocyte count
Treatment-Emergent Malignancies
With up to 7 years’ follow-up, treatment-emergent malignancies among ozanimod-treated patients with MS were 324.8 per 100,000 person-years.22 According to the national Institutes of health (NIH) Surveillance, Epidemiology and End Results database for 2021, the frequency of “cancer of any site” among the general US population was 446 per 100,000 person-years.25 Malignancies, such as melanoma, basal cell carcinoma, squamous cell carcinoma, breast cancer, seminoma, cervical carcinoma, and adenocarcinomas, including rectal adenocarcinoma, were reported with ozanimod in controlled trials.14 In DAYBREAK, the incidence of malignant melanoma, non-melanoma cutaneous malignancies, and non-cutaneous malignancies was 6.3, 107.1,and 194.8 per 100,000 person years, respectively.26
Pregnancy
There are no adequate and well-controlled studies in pregnant women.Based on animal studies, ozanimod may cause fetal harm.14 Women of childbearing potential should use effective contraception during treatment and for 3 months after stopping ozanimod.14 In SUNBEAM and RADIANCE Phase III trials, patients were required to discontinue ozanimod if pregnancy was confirmed, unless they elected to terminate the pregnancy, in which case they were permitted to continue ozanimod. Male patients were to notify the investigator if their female partner became pregnant.14,19,21 in a total of 82 pregnancies, of which 57 were in patients with relapsing MS, all patients discontinued ozanimod in the first trimester. There were 44 (53%) live births, 39 (88.6%) of which were normal infants and four (9.1%) of which were premature births (11% for the general population).27 There has been no increased incidence of fetal abnormalities or adverse pregnancy outcomes.27 Rates of 12 spontaneous abortions (14.5%) and one duplex kidney (2.3%) were consistent with the general population (18-31% and 1.8%, respectively).27 Readers are directed to the important safety information at the end of this article for further information on fetal risk. For additional safety information, please see the full Prescribing Information and Medication Guide linked at the top of this article.
Rebound
Berkovich discussed the issue of rebound,1 which she described as the return of MS activity and/or severe exacerbation of disease or severe persistent increase in disability after treatment discontinuation. Rebound is a key concern for clinicians and patients, notably when symptoms are ”above and beyond just the return of MS activity,” as has been reported with fingolimod.1 Shin noted that, with ozanimod, “what is not seen is the kind of rebound …that we had seen with some other agents.” Findings from the DAYBREAK OLE study support this observation, where no patients experienced disease rebound, and only 3.3% (n=55/1,679) of patients experienced relapse after ozanimod discontinuation.28 Most relapses (98%; n=54/55) were mild or moderate, 2% (n=1/55) occurred while the patient was using a DMT, and 76% of patients made a full recovery.28
Real-World Evidence
In the DAYBREAK OLE study, ozanimod demonstrated a low discontinuation rate of 3.9% due to aes across a follow-up period of up to 7 years
Also to be considered:
Ozanimod is an S1P receptor modulator that is structurally distinct from the first-generation treatment, fingolimod, and binds with high affinity to S1P1 and S1P5.1,10,14 As Berkovich noted, the “pharmacological representatives of the same class are not the same,” distinguishing ozanimod’s structural distinction within the S1P modulator class.
Ozanimod has demonstrated comparable safety to platform therapy IFN β-1a.14,19,21 Long-term data showed that 15.3% of patients reported serious infections, 9.6% reported severe infections, and 3.9% of patients discontinued due to TEAEs.22 Furthermore, treatment-emergent malignancies occurred in 324.8 per 100,000 person years.22,24 Its once-daily management,coupled with a demonstrated safety and efficacy profile,show that ozanimod might potentially be an appropriate oral DMT for early treatment of patients with RMS. Berkovich added a patient-centered perspective: “When a patient leaves your office, they should feel better as compared to how they came…that is what realistically we can see with adequately treated patients.”
IMPORTANT SAFETY INFORMATION
INDICATION
ZEPOSIA® (ozanimod) is indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
Contraindications:
- Patients who in the last 6 months,experienced myocardial infarction,unstable angina,stroke,transient ischemic attack (TIA),decompensated heart failure requiring hospitalization,or Class III/IV heart failure or have a presence of Mobitz type II second-degree or third-degree atrioventricular (AV) block,sick sinus syndrome,or sino-atrial block,unless the patient has a functioning pacemaker
- Patients with severe untreated sleep apnea
- Patients taking a monoamine oxidase (MAO) inhibitor
Infections: ZEPOSIA may increase the susceptibility to infections. Life-threatening and rare fatal infections have occurred in patients receiving ZEPOSIA. Obtain a recent (i.e., within 6 months or after discontinuation of prior MS therapy) complete blood count (CBC) including lymphocyte count before initiation of ZEPOSIA. Delay initiation of ZEPOSIA in patients with an active infection until the infection is resolved. Consider interruption of treatment with ZEPOSIA if a patient develops a serious infection. Continue monitoring for infections up to 3 months after discontinuing ZEPOSIA.
- Herpes zoster and herpes simplex were seen in clinical trials of ZEPOSIA. herpes simplex encephalitis and varicella zoster meningitis have been reported with sphingosine 1-phosphate (S1P) receptor modulators. Patients without a healthcare professional-confirmed history of varicella (chickenpox),or without documentation of a full course of vaccination against varicella zoster virus (VZV),should be tested for antibodies to VZV before initiating ZEPOSIA.
- Cases of fatal cryptococcal meningitis (CM) and disseminated cryptococcal infections have been reported with S1P receptor modulators. If CM is suspected, ZEPOSIA should be suspended until cryptococcal infection has been excluded. If CM is diagnosed, appropriate treatment should be initiated.
- In clinical studies, patients who received ZEPOSIA were not to receive concomitant treatment with antineoplastic, non-corticosteroid immunosuppressive, or immune-modulating therapies used for treatment of MS. concomitant use of ZEPOSIA with any of these therapies would be expected to increase the risk of immunosuppression. When switching to ZEPOSIA from immunosuppressive medications, consider the duration of the
ZEPOSIA: Potential Cardiovascular Effects
Treatment with ZEPOSIA (ozanimod) can lead to an increase in blood pressure, typically observed after approximately three months of therapy, and this elevation persists throughout the treatment duration. Regular blood pressure monitoring and appropriate management are crucial for patients taking ZEPOSIA.
The precise mechanism for this blood pressure increase isn’t fully understood, but it necessitates careful observation. Clinicians should proactively monitor patients and adjust antihypertensive medications as needed to maintain blood pressure within a healthy range. This is particularly important for individuals with pre-existing hypertension.
For example, a clinical trial participant with baseline blood pressure of 120/80 mmHg experienced a sustained increase to 135/85 mmHg after four months on ZEPOSIA, requiring an adjustment to their existing lisinopril dosage. This information is detailed in the ZEPOSIA prescribing information (FDA).
Respiratory Function and ZEPOSIA
ZEPOSIA may cause a reduction in pulmonary function. Healthcare providers should consider performing spirometric evaluations to assess respiratory function during treatment, especially if clinically indicated by patient symptoms or medical history.
The decline in pulmonary function is thought to be related to the drug’s mechanism of action, affecting lymphocyte trafficking and potentially impacting lung tissue. Spirometry, a common lung function test, measures the amount of air a person can inhale and exhale, and the speed of exhalation. This allows for early detection of any meaningful changes.
the FDA-approved label for ZEPOSIA recommends clinical judgment be used to determine the necessity of spirometric testing based on individual patient factors.
Macular Edema Risk with ZEPOSIA
S1P modulators, the class of drugs to which ZEPOSIA belongs, carry an increased risk of macular edema, a swelling of the macula in the eye that can lead to vision loss. A baseline fundus examination, including evaluation of the macula, is recommended before initiating ZEPOSIA therapy.
Macular edema occurs when fluid accumulates in the macula, the central part of the retina responsible for sharp, central vision. Early detection is critical because prolonged macular edema (lasting six months or more) can result in permanent visual impairment. Regular fundus examinations, including assessment of the macula, are essential during treatment and whenever a patient reports changes in vision.
Patients with a history of uveitis or diabetes mellitus are at a heightened risk of developing macular edema while on ZEPOSIA. The complete prescribing information advises considering discontinuation of ZEPOSIA if macular edema develops, as the risk of recurrence upon re-challenge is currently unknown.
