Japanese research group “Correcting immune T cell defects from genetic diseases using CRISPR genetic scissors”
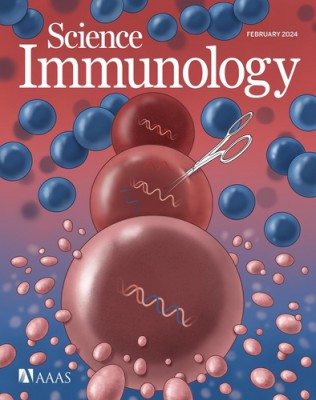
Preclinical experiments to correct genetic defects that cause immune diseases using CRISPR-Cas9, a gene editing technology, have been successful in human and mouse cells.
Dr. Klaus Lazeski’s team from the Max-Delbrück Center for Molecular Medicine of the Helmholtz Society in Germany reported on the 5th in the scientific journal Science Immunology that they have corrected defects in the immune system’s memory T cells in mouse models of the genetic disease using CRISPR genetic scissors and to have treated 2 children with genetic diseases. It was also revealed that the effect was confirmed in cellular experiments using human blood.
Genetic defects can cause a fatal overactive immune response. In this study, the research team explored the possibility of a gene-correction treatment for familial erythrophagocytic lymphohistiocytosis (FHL), a rare immune system disease that occurs in children younger than 18 months.
FHL is a fatal disease caused by a genetic mutation that prevents the normal functioning of the immune system’s cytotoxic T cells, which kill cells infected by the virus.
In this disease, even when infected with Epstein-Barr virus (EBV), cytotoxic T cells are unable to eliminate infected cells and the immune response rapidly increases, resulting in a cytokine storm and excessive inflammatory response. It can be treated with hematopoietic stem cell transplantation (HSCT), but the mortality rate is high, so effective treatment is needed.
In this study, the research team developed a method to correct T cell defects in EBV infection model mice using adeno-associated virus (AAV)-based CRISPR gene scissors.
First, the genes of EBV infection model mice were manipulated to prevent T cells from producing a protein (perforin. Prf1) that kills infected cells. Perforin deficiency is a common genetic defect in patients with familial erythrophagocytic lymphohistiocytosis.
When a state similar to EBV infection was induced in mice with a defect in the perforin gene, cytotoxic T cells failed to eliminate it and the immune response occurred in excess, resulting in hemophagocytic lymphohistiocytosis.
The research team then collected memory T stem cells from the blood of these mice, corrected the perforin gene in the T cells with CRISPR genetic scissors, and then injected them back into the mice.
As a result, the corrected T cells functioned normally, the excessive immune response calmed down, and the mouse recovered from hemophagocytic lymphohistiocytosis.
In addition, blood was collected from two patients, including a child with a defect in the perforin gene, and CRISPR gene editing technology was applied to the T cells. Test-tube experiments confirmed that the corrected T cells restored normal function.
This means, according to the research team, that the treatment is effective in principle, but before applying it to patients it is necessary to resolve some unanswered questions and verify the effectiveness and safety through clinical trials.
Dr. Lazeski said: “This procedure is minimally invasive, requires only a small amount of blood and, unlike bone marrow transplantation in mice, requires no preparatory treatment. This treatment represents a revolutionary breakthrough in the treatment of familial erythrophagocytic lymphohistiocytosis “I hope it happens,” he said.
◆ 출처: Science Immunology, Klaus Rajewsky et al., “Precise CRISPR-Cas9 Gene Repair in Autologous Memory T Cells to Treat Familial Hemophagocytic Lymphohistiocytosis,”
<저작권자(c) 연합뉴스>
#Successful #preclinical #experiment #correcting #genetic #diseases #defective #genes #human #mouse #cells #Donga #Science